Core Competencies for Healthcare Leaders (Part 1)
MHA Search
For the 2023-2024 academic year, we have 112 schools in our MHAOnline.com database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
The healthcare sector exists at a transformative juncture of massive proportions. As newly emerging leaders enter and rise up within this field, they will need to bring with them an ever-growing and diverse set of skills and a large body of knowledge. This turbulent environment is being rapidly shaped by technological advancements, evolving patient expectations, regulatory changes, and a global emphasis on public health sharpened by the Covid-19 pandemic turned endemic.
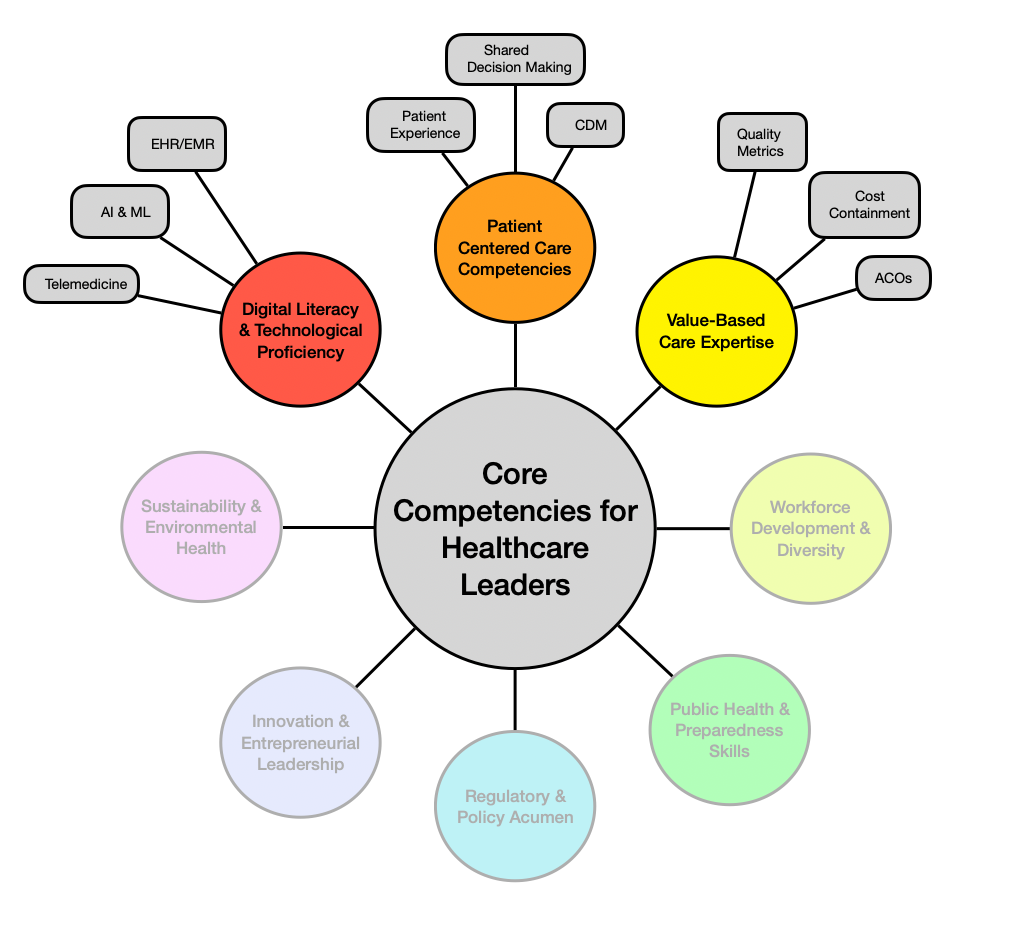
Mastering the skills needed to effectively navigate and manage the people, processes, and tools at play is crucial for gaining and retaining a competitive edge. This three-part essay series summarizes important areas where rising healthcare leaders should focus their efforts as they develop their essential skills and build out their knowledge base. This first essay will cover digital literacy & technological proficiency, patient-centered care competencies, and value-based care expertise. The remaining topics illustrated in the competency chart will be covered in future writings of the series.
While this collection is comprehensive, it is certainly not complete. Any one of these areas of focus constitutes a field of study in its own right, replete with experts, opinion leaders, research, critiques, analysis, and debates between warring factions. Healthcare leaders will benefit from a continuous and comprehensive approach to learning throughout their careers.
Digital Literacy and Technological Proficiency
Digital transformation is reshaping healthcare delivery and management—but it is also quite a broad term. It refers to the understanding of the interplay between technologies used in healthcare and how those influence and promote perspectives towards the concept of innovation within the healthcare sector—which in turn shifts more resources toward the technology development, and the cycle continues in perpetuity (though neither smoothly nor steadily).
In short, healthcare leaders need to develop and maintain their robust understanding of advanced technologies to implement them effectively and drive innovation continuously. The three most common applications right now are:
Proficiency in Artificial Intelligence and Machine Learning
Providers and their healthcare organizations (HCOs) must become comfortable leveraging the power of machine learning algorithm-driven tools to enhance their diagnostic accuracy, tailor treatment plans, and forecast patient outcomes for individuals and populations.
Artificial intelligence applications must be explored to increase efficiency and reduce errors within many common operational processes and activities of administrative staff. Leaning on the strengths and developing processes that consider these technologies’ limitations is paramount. Whenever possible, a pilot rollout should be undertaken to refine protocols and workflows before more widespread adoption.
Expertise in Telemedicine
The explosive rise of telemedicine tools and programs from the pandemic fundamentally shifted many healthcare interactions into the digital realm for the long haul. This ongoing integration of digital and in-person care necessitates that leaders ensure providers and support staff alike achieve mastery of the chosen telehealth platforms to ensure as seamless a patient experience as possible.
Leaders are responsible for developing policies that promote digital literacy and recognize and work to reduce access disparities within target populations. Leaders should strive to continuously enhance telehealth services with the overarching goals of increasing overall accessibility and improving patient satisfaction scores.
Mastery of the Electronic Health Record (EHR)
EHR and electronic medical record (EMR) systems have been fairly widespread for decades, particularly among the larger HCOs. These software systems streamline the care continuum from encounter record-keeping through revenue cycle management.
As they have grown much more complex and externally connected to much larger patient data repositories, they are increasingly being used in more sophisticated ways. These include improving coordination among different healthcare providers (even from entirely distinct HCOs), enhancing patient outcomes (often with some support from ML- and AI-powered tools), and even taking the first steps toward precision medicine for the masses.
Leaders are responsible for facilitating seamless integration of EHR systems, prioritizing interoperability for both operational and regulatory purposes, and of course, enforcing appropriately robust cybersecurity measures to protect patient data and the reputation of the HCO and its providers.
Patient-Centered Care Competencies
Patient-centered care is a broad concept that describes an overarching care strategy of:
- Focusing on involving patients in their healthcare decisions
- Tailoring services to meet their individual needs and preferences
The concept is deceptively simple on paper, but the distorted and often contradictory incentives structure of the sector (i.e., sometimes we treat healthcare as a right, and other times we treat it as a business) render the practices maddeningly complex. Leaders must focus substantial efforts to promote this approach in any meaningful way effectively.
Shared Decision-making Facilitation
Leaders play a key role in designing the policies and processes that allow for and promote shared decision-making. This practice intends to engage patients and healthcare providers in a collaborative decision-making process that respects autonomy and liability. These discussions necessitate outstanding communication skills, a flexible perspective, and the ability to educate patients in meaningful terms to provide care that is both collaborative and personalized and constitutes “good medicine.”
Enhancing Patient Experience
Enhancing the patient experience involves reducing wait times, improving communication, and providing compassionate care, among other metrics. Several national surveying tools have been gathering and sharing these scores with hospitals, providers, HCOs, and healthcare leadership for decades. While many of the measured variables remain highly relevant, newly emerging technologies and evolving expectations render these traditional tools incomplete.
Leaders must implement strategies to measure and improve patient satisfaction that are regularly revised to reflect the impact of technological integrations while still employing data-driven approaches and robust statistical analysis to assess these patient experiences.
Chronic Disease Management
As the cost burden of chronic disease management (CMD) begins to encounter the financials of outcomes-based care and value-based care contracts for payment, success metrics are no longer limited to dollars. Healthcare leaders must prioritize developing and implementing integrated care models involving multidisciplinary teams of medical providers, scalable programs for patient education, and tools and workflows that leverage continuous monitoring technologies. Effective chronic disease management is essential for improving patient outcomes and reducing healthcare costs.
Value-based Care Expertise
Value-based care (VBC) refers to a type of reimbursement structure in which various states of patient health conditions are quantified, in addition to the more traditional cost calculations of providing the care to achieve them. In short, VBC emphasizes outcomes and cost-efficiency over volume. While this explanation is fairly oversimplified, leaders must dive in far deeper to gain an adequate understanding of these incentive structures to manage these types of contracts proficiently. This requires much longer-term financial planning and coordination with clinical leadership, billing, and information technology leaders in an iterative and continuous process.
Mastery of Quality Metrics
Leaders need to be adept at understanding and utilizing quality metrics such as patient outcomes, readmission rates, and patient satisfaction. They must gain fluency in this language in terms that are meaningful to clinical leadership to align incentives for providers among all specializations and resolve competing interests through physician-led forums with transparent rule-making and revisions. Implementing quality improvement initiatives to meet and surpass these benchmarks is crucial for thriving in a value-based care environment.
Leaders also should be mindful that data alone cannot tell the whole story and that physician leadership must be empowered to play an appropriate leading role for their respective clinician teams.
Cost Containment Strategies
Rising healthcare costs demand leaders devise strategies to reduce expenses without compromising quality. This aggravatingly broad goal has been touted within the healthcare sector for as long as anyone can remember, but never before has the pace of change been as great as it is now, which has greatly rendered the sentiment far more tangible to leadership.
The basics of cost containment strategy are well covered in any MHA program curriculum, and many MBA programs. In the broadest terms, they include optimizing resource allocation, minimizing unnecessary tests and procedures, and leveraging technology to enhance efficiency.
Knowledge of Accountable Care Organizations (ACOs)
Leaders must be well-versed in the structure and function of ACOs, which aim to provide coordinated care to Medicare patients while reducing costs and improving quality. The incentives structure is very similar to VBC arrangements, but with a public funding source and more publicly available performance metrics. Understanding the financial and clinical implications of ACO participation is essential.
Conclusion
Emerging and rising healthcare leaders must acquire and maintain a diverse set of skills and a wide base of knowledge to successfully navigate a rapidly evolving landscape. Each of the three cores explored in this first writing—digital literacy & technological proficiency, patient-centered care competencies, and value-based care expertise—contains a multitude of applications, all of which have far-reaching impacts and require coordinating various stakeholders both internal and external to the organization.
Leaders in the field must remain adaptable, forward-thinking, and committed to continuous learning and improvement – for themselves, their teams, and the patients they serve. The future of healthcare leadership depends on their ability to respond to these challenges and seize opportunities that will enhance the quality and equity of care.
It can seem daunting, but by mastering these skills (particularly through MBA/MHA programs), leaders can build successful careers and—importantly—significantly impact healthcare delivery and outcomes, positively impacting millions of lives in the process.

