Core Competencies for Healthcare Leaders (Part 3)
MHA Search
For the latest academic year, we have 170 schools in our MHAOnline.com database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
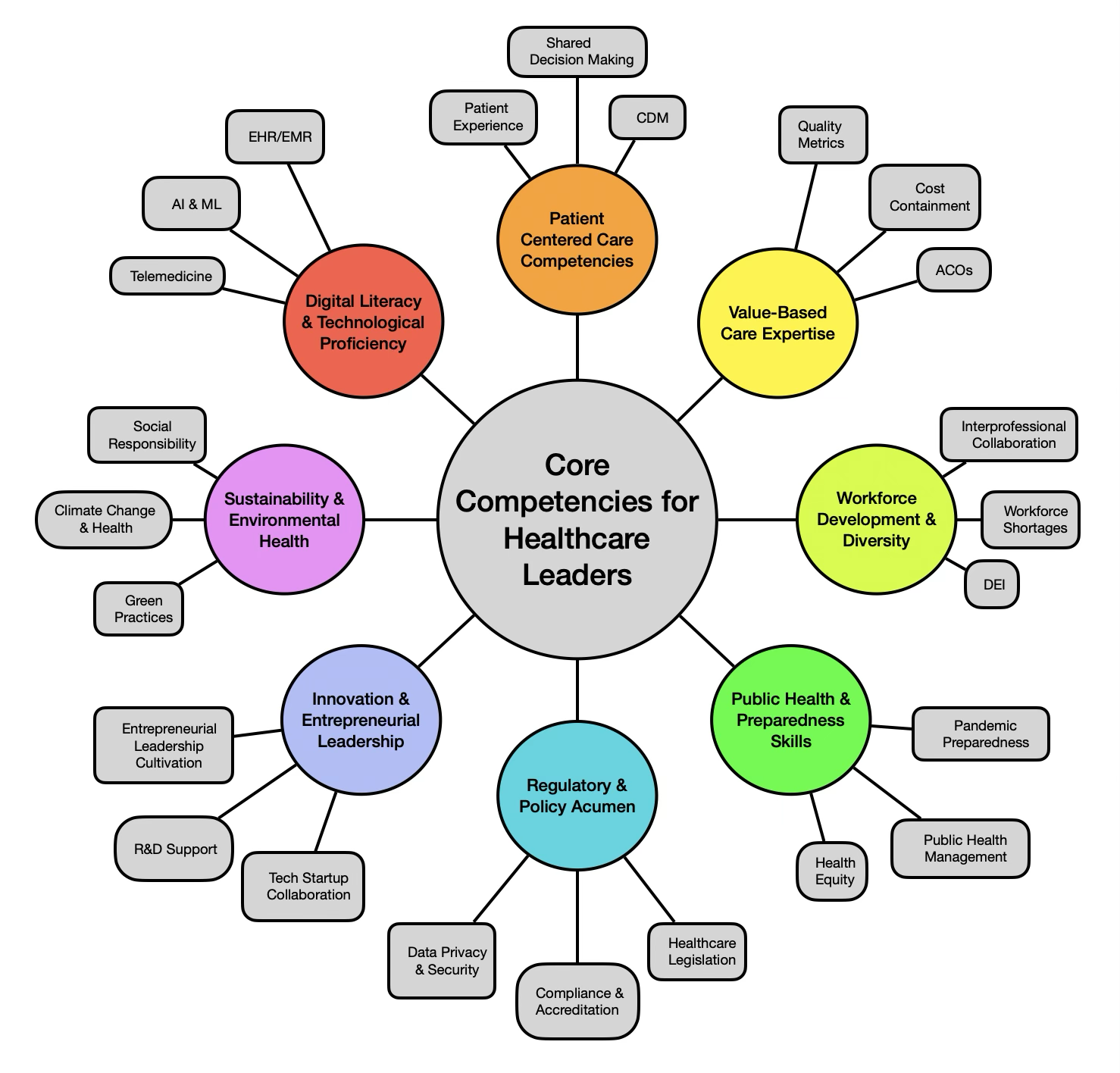
In part one of this three-part series, we covered the competencies of digital literacy and technological proficiency, patient-centered care, and value-based care expertise. This cluster focused heavily on pragmatic applications that leverage data and technologies in the provision of clinical care.
In our second piece, our focus shifted outward, taking a broader view of the sector by examining the competencies of workforce development and diversity, public health and preparedness, and regulatory and policy acumen.
This third and final piece on core competencies for rising healthcare leaders covers the final two circles in the organizational graphic below. Here, we turn our eyes toward the future of the sector, diving into the competencies of innovation and entrepreneurial leadership, as well as sustainability and environmental health.
Innovation and Entrepreneurial Leadership
Innovation and entrepreneurship have always driven advancements in the healthcare sector, though the increasing pace of change over the past decade—largely driven by rapid digitalization—may make it seem like a newer attribute. Today’s healthcare leaders must have the skills to foster a culture of innovation that embraces an entrepreneurial approach in a way that is both safe and value-adding
The key to walking that fine line lies largely in careful management of project scope. This allows reasonable management of risk—an essential responsibility of any healthcare leader—without eliminating opportunities to leverage new approaches, tools, and technologies.
Collaborating with Health Tech Startups
Effective leaders know their limitations and strengths. At the intersection of healthcare and technology startups, partnerships generally yield more favorable results than attempting to master all aspects alone. Leaders must be open to collaborating with health tech startups to benefit from innovative solutions with powerful technological capabilities. Developing these partnerships requires both operational and risk management skills.
While healthcare and technology partnerships may feel riskier than those in other sectors due to the stakes involved in people’s health and well-being, they are increasingly necessary for the survival of health systems and the healthcare sector as a whole. Leaders must be prepared to take appropriate risks to foster short- and long-term innovation.
Supporting research and development (R&D) initiatives and encouraging participation in clinical trials and translational research are critical. Skills in project management and research administration are crucial for advancing medical knowledge and improving patient care.
Supporting Research and Development
R&D in healthcare encompasses various activities. One of the most prominent is “academic medicine”—the blending of clinical activity and medical research, supported by institutional resources and safeguards. This is typically physician-led, with support from doctoral candidates and research staff, and often relies on clinical patient populations.
This type of R&D is considered prestigious for physicians, rooted in longstanding medical institutions, which today often consist of large health systems coupled with medical schools. Funding is heavily supported by both public and private grants, with the largest portion of public funding usually coming from the National Institutes of Health (NIH). Private and institutional trust funding also help cover research costs and to attract notable faculty, which in turn perpetuates success in securing grants.
Healthcare leaders may find themselves in charge of a provider group with responsibilities split between clinical and research affairs, which may, at times, generate incentives that are not entirely aligned and must be carefully handled.
Another significant cluster of R&D activity in healthcare is sponsored by pharmaceutical or “life sciences” companies. Unlike academic medicine, this falls into the private sector. There can be overlap between the two, with life sciences companies funding research at prestigious institutions.
However, this has limitations and risks, such as restricting research to drugs produced by that company and raising concerns about bias in findings. The appearance of bias can be damaging to both researchers and their institutions, making this funding source less preferable and less prestigious due to the potential cost of damaged patient perception.
Development encompasses not only new drugs, protocols, and approaches to care, but also the training of new physicians, advanced practitioners, and research scientists within teaching hospitals. Healthcare leaders must familiarize themselves with all of these areas and seek opportunities to participate, promote, and leverage potential value-added benefits for their teams and the patient populations they serve.
Cultivating Entrepreneurial Leadership
Entrepreneurial leadership involves taking calculated risks, being adaptable, and fostering a culture of innovation. Emerging leaders should cultivate these skills within themselves to navigate the complex and rapidly changing healthcare environment effectively. Additionally, leaders must promote the development of entrepreneurial skills within their teams, which becomes increasingly important as they advance through the organizational hierarchy and begin managing leaders who are managing teams themselves.
Sustainability and Environmental Health
The past decade has seen a significant shift in the healthcare sector’s approach to sustainability, from largely reactive to decidedly proactive. Sustainability can refer to the long-term financial health and viability of an institution. The increasing ease of data access and analysis has imposed upon healthcare leaders the additional responsibility of planning for a future that will only arrive long after they have risen to higher levels of management. They must increasingly demonstrate this planning with data-driven projections.
Sustainability also encompasses an organization’s impact on the environment. This not only carries institutional risks from potentially irresponsible environmental practices but also affects the local population’s health—the same population that comprises the organization’s patient base. While this connection may initially seem far-fetched and hard to quantify, it becomes more relevant in the growing proportion of value-based and outcomes-based care contracts within a healthcare organization’s payer mix.
In all of these cases, it is clear that leaders need the skills to implement sustainable practices and address the health impacts of climate change within the scope permitted by their roles. The “negative externalities” of classical monetary economics are no longer theoretical but are evolving into distinct line items on profit and loss statements for which leadership will be held accountable.
Implementing Green Healthcare Practices
To take ownership of green practices, leaders must prioritize sustainability initiatives, such as energy-efficient buildings, waste reduction, and sustainable procurement for supplies and materials. Skills in environmental management and sustainability are essential for reducing the environmental footprint of healthcare organizations.
A growing number of master of health administration (MHA), master of public health (MPH), and master of business administration (MBA) programs now include coursework dedicated to training leaders on these practices. Additionally, there is a growing sub-sector of companies offering expert consultation and support in assessing and improving metrics of waste and environmental impact without sacrificing short-term profitability.
Addressing Climate Change and Health
Even healthcare leaders who have reached the peak of their careers often feel helpless in the face of climate change. However, this does not justify inaction. Making a difference begins with understanding the science and policies behind climate change. Opportunities must be pursued to shift the debate from emotionally charged rhetoric to thoughtful discussions based on reliable data.
Leaders at all levels can help address the health impacts of climate change by advocating for policies that mitigate environmental risks and promote resilience in healthcare infrastructure. Adequate skills in policy advocacy are crucial for addressing these challenges.
Promoting Social Responsibility
The final aspect of the core competency of sustainability and environmental health is promoting social responsibility. Healthcare organizations are responsible for contributing to the well-being of their communities—patient communities are, after all, served by the institution and its staff. Social responsibility is an act of service, not just rhetoric.
Leaders should engage in initiatives such as community outreach programs and support the development and dissemination of health education and accessibility information. The distribution of vital information should leverage the networks that have grown from the proliferation of consumer technologies and smart devices. Healthcare involvement with patients should increasingly be integrated into daily life, as empowering patients is socially responsible and more cost-effective than historically reactive approaches. Skills in community engagement and public health promotion are essential for these efforts, while expertise in gamification and user experience research can greatly enhance them.
Conclusion
This final segment of our series underscored the importance of forward-thinking leadership that balances risk with opportunity, supports the growth and development of their teams, and demonstrates a commitment to the health and well-being of communities and the environment.
As the healthcare landscape continues to evolve rapidly, leaders must be equipped with diverse competencies to navigate its complexities and uncertainties effectively. From fostering innovation through entrepreneurial leadership to embracing sustainability and environmental stewardship, today’s healthcare leaders are called to address both the immediate needs of their organizations and the broader societal challenges ahead. By integrating these competencies into their practice, rising healthcare leaders can drive meaningful progress in a field that is fundamental to the vitality of society.

