Core Competencies for Healthcare Leaders (Part 2)
MHA Search
For the 2023-2024 academic year, we have 112 schools in our MHAOnline.com database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
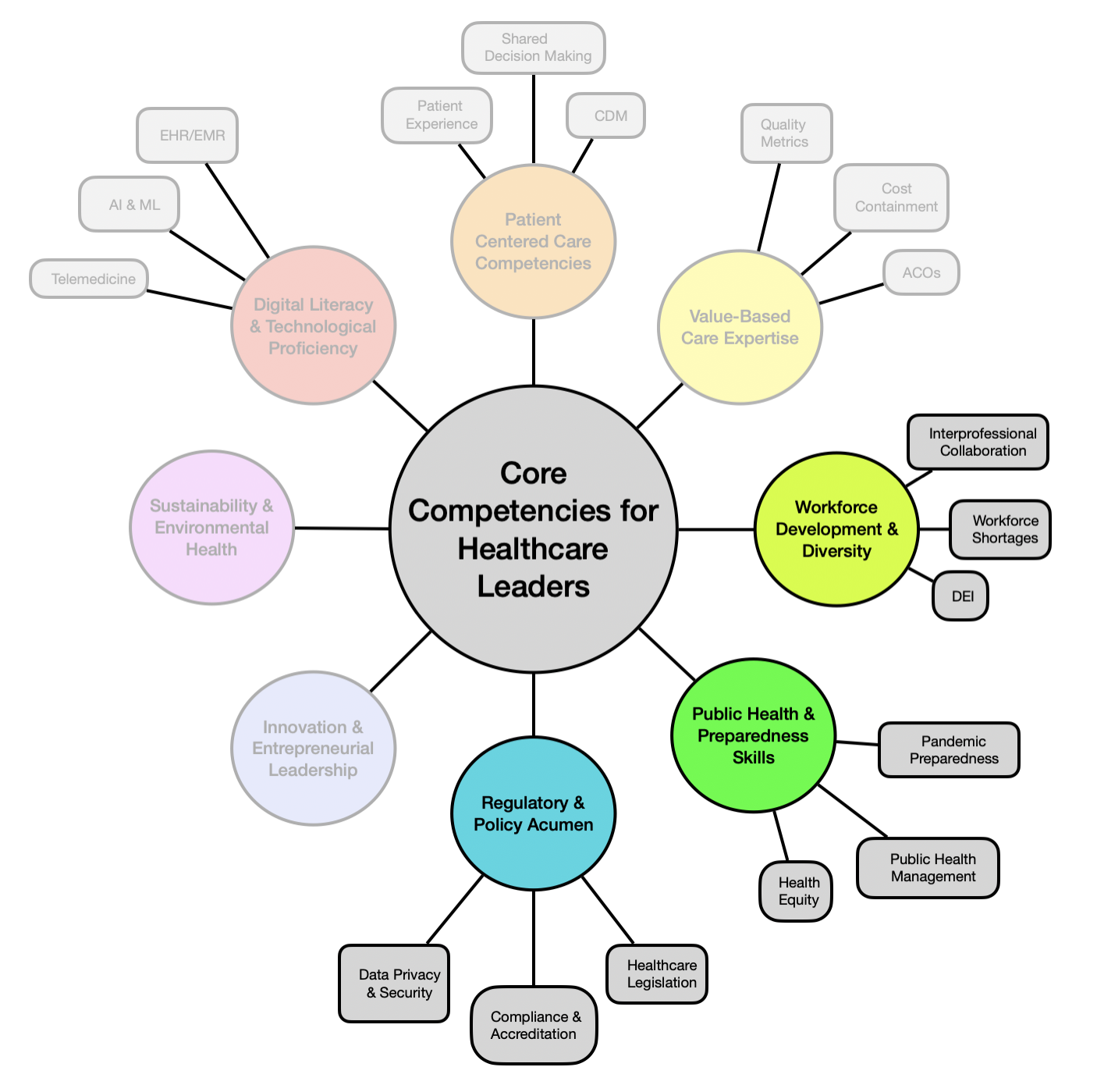
In the first essay of this three-part series, we covered the core competencies of digital literacy and technological proficiency, patient-centered care, and value-based care expertise.
In this second piece, we will continue rounding the chart below and cover workforce development and diversity, public health and preparedness skills, and regulatory and policy acumen.
As thoroughly emphasized in part one, it is crucial for healthcare leaders to remain adaptable, forward-thinking, and committed to continuous learning and improvement for themselves, their teams, and their organization as a whole. Future success will depend on their ability to respond to unexpected challenges in a way that leverages all possible opportunities. We hope that this framework helps support emerging leaders by illuminating an energizing landscape upon which one can build a career path.
Workforce Development and Diversity
A capable and diverse workforce is critical for any large enterprise to thrive, regardless of its economic sector. Evolving demographics, a highly interconnected global economy, and the ever-present communication web of social media and information movement have strengthened the importance of institutional integrity. This means genuinely honoring commitments to diversity—not merely giving lip service.
A diverse and well-supported workforce is vital for delivering high-quality care and fostering innovation that can disseminate from both the top down and the bottom up. Leaders need well-honed skills and a thoughtful approach to develop, manage, and support their teams using these practices as central pillars.
Interprofessional Collaboration
One of the most powerful tools that healthcare leaders have in their toolkit is the opportunity to leverage interprofessional collaborations. Interprofessional collaboration strategies promote comprehensive and coordinated care for patient populations throughout the care continuum. Value gains stem from facilitating meaningful collaboration among doctors, nurses, pharmacists, information technology professionals, coverage specialists, researchers, social workers, and many more.
Importantly, interprofessional collaboration can also provide an opportunity for individuals from historically less advantaged groups to begin building the types of professional relationships that are critical to reaching the highest levels of leadership within an organization. This promulgates diversity up through the chain of management in a more organic way. Leaders should feel confident that the investment of their time in establishing and checking-in with these relationships and channels/forums for communication will pay for itself many times over.
Addressing Workforce Shortages
Working closely with human resource executives, leaders will benefit tremendously from a proactive approach for developing strategies to recruit, retain, and support healthcare professionals amid workforce shortages, which can be devastating to the financial viability of HCOs of all sizes.
The pandemic provided a crash course for many leaders in just how devastating a lack of preparedness can be, which also cannot be solved overnight. This is particularly so when a primary driver for the labor shortage is burnout—a complex phenomenon that can be triggered by leadership that has not been well attuned to the evolving needs of their staff. Thus, it is clear that effectively addressing workforce shortages means in large part proactively developing preventative measures that will retain staff before shortages become detrimental to operations,
in addition to recruitment strategies. Many leaders have begun relying on data to better meet the needs of their teams in a cost-effective way; one increasingly common example is using predictive algorithms that optimize staffing schedules.
Diversity, Equity, and Inclusion (DEI) Initiatives
Diversity, equity, and inclusion (DEI) initiatives are programs and activities intended to foster an inclusive environment, which is a workspace that respects and values diverse backgrounds and perspectives. This broad definition has more than once resulted in initiatives that sound meaningful and allow leaders to check a box but do little else beyond frustrate staff. Indeed, there are few ways to more rapidly degrade worker commitment to an organization than engagement with poorly designed DEI initiatives.
Not surprisingly, building and implementing effective DEI initiatives using limited resources takes a lot of work. But leaders are advised to not shy away from trying simply because they fear they may fail. Humility and self-education can go a long way in overcoming initial discomfort—there are a growing number of resources that support healthcare leaders in learning how to better address implicit biases for themselves and within their teams.
An increasing number of companies and non-for-profit groups can provide DEI training materials and program tools to support leaders in rolling out DEI initiatives. Those well-executed initiatives will naturally align with the aforementioned practices of interprofessional collaborations and mitigating staff shortages, and this powerful trifecta can help leaders achieve measurable and continuous improvement in their development and diversity goals.
Public Health and Preparedness Skills
The Covid-19 pandemic underscored the importance of public health and preparedness skills for healthcare leaders and their organizations. This begins with the population served by the HCO and expands via information exchange with other institutions, regulatory and legislative bodies, and the public at large. The information exchanged is often centered on best practices, health outcomes, and other information relevant to public health goals.
Public health preparedness also envelopes the much more mundane but just as important arm of proactive inventory management. Many HCOs have realized the importance of cultivating relationships with their suppliers, and learning how they are impacted by possible disruptions and shocks to global supply chains, as part of a better strategy to reduce risk of supply shortages.
Pandemic Preparedness
At the earlier stages of the pandemic, care facilities, hospitals, clinics, and research institutions collaborated and shared their data on what was (and was not) working to treat Covid-19 patients in unprecedented ways—ways that also required a temporary suspension of HIPAA enforcement.
Leaders today must develop robust response plans for future pandemics and public health emergencies that are compliant with privacy and safety regulations. This includes ensuring adequate supplies of personal protective equipment (PPE) and investing in public health infrastructure, including investments that build and implement channels for communication to and from the public.
Effective communication channels can leverage existing networks and technology while providing HCO leadership with an effective mechanism to ensure timely communication of messages and important health information. Public trust in healthcare institutions and public health officials was substantially eroded from poorly coordinated communication during the pandemic, and this trust must be rebuilt for the sector’s future success. This will take time, resources, and—most importantly—enthusiastic support from rising leaders within healthcare.
Population Health Management
Collaboration for the good of the public does not require a pandemic crisis in order to occur. The exchange of healthcare information and research findings is the primary driver for medical conferences and related events. When healthcare leaders present at such events, it is often in partnership with the physicians or other providers directly involved with said patient populations, as well as IT and research analytics leadership who have provided support on the number crunching. Digital dissemination of this information can and should take place to supplement larger events, and to keep information up to date, in a transparent and collaborative process.
Leaders can then take these learnings back to their own institutions, to implement relevant health initiatives that can improve community health and reduce healthcare disparities in their patient populations. Skills in addressing social determinants of health, promoting preventive care, and managing chronic conditions are essential to effectively apply concepts learned from a conference into a successful clinical program. Leaders are advised to strengthen relationships with clinician leadership and to pursue a data-driven approach to pilot programs to increase chances of roll-out success.
Health Equity Advocacy
There is a growing public sentiment for HCOs to play a leading role in addressing the societal challenge of health inequities. This is likely due to health outcomes and their overlap with the value-based care models of reimbursement that make up a growing proportion of large HCO contracts. Of course, moving the needle on health inequity will require legislation to ensure that HCOs get access to the resources needed to operate in coordination with complimentary social programs and initiatives that aim to achieve similar goals.
Leaders should advocate for policies that promote access to care and reduce socioeconomic barriers for patients, in a way that is within the scope of their role. Skills in health equity advocacy and community engagement experience are powerful tools for addressing health disparities and promoting equitable healthcare, but these are lofty goals indeed.
Leaders taking their first steps in this area may appreciate an approach of joining groups where these conversations are taking place, and becoming familiar with the language, terms, and history of such discussions.
Regulatory and Policy Acumen
Healthcare leaders must stay informed about regulatory and policy changes that impact the industry. Larger HCOs will have a dedicated department for regulatory and compliance requirements, while smaller organizations tend to distribute accountability of these requirements among division leadership posts.
Whether large, small, or in-between, every organization puts itself and its patients at risk if these regulations are not strictly followed, or if protocols are carelessly designed and open the door for errors and oversights.
Understanding Healthcare Legislation
In larger HCOs, lobbying for (or against) the enactment of certain legislation can be a substantial use of resources—but this is reasonable, given the potentially profound consequences for the institution. As with all things politics, it can become quite tempestuous; arming oneself with a historical perspective and learning stakeholder perspectives can help reduce this at least slightly.
For rising leaders, a terrific place to begin is reviewing the history of healthcare-specific legislation and learning from the historical perspectives the how and why behind previous regulations. This helps not only develop the language needed to understand and effectively discuss healthcare policies but also gain more nuanced insights into these debates and be better able to plan ahead for future regulatory rollouts.
Compliance and Accreditation
Leaders must ensure that their organizations meet all regulatory requirements and accreditation standards without fail. Knowledge of specific processes and protocols for up-to-date compliance management and quality assurance is a must for maintaining accreditation and avoiding penalties. Detailed documentation should be reviewed at regular intervals and made readily available for unexpected compliance spot checks.
Data Privacy and Security
With the rapid implementation of increasingly complex digital health technologies, digital privacy and security are some of the relatively newer competencies that are critical for the success of any rising healthcare leader. Leadership must go far beyond merely following the Health Insurance Portability and Accountability Act (HIPAA) guidelines, and maintaining oversight on Protected Health Information (PHI) material.
Now, leaders must develop strong relationships with IT leadership and work closely to develop and implement robust data protection measures that coordinate with provider and staff protocols. Skills in cybersecurity and data privacy management are essential to not only comply with regulatory requirements but also increasingly protect the reputation of the healthcare organization.
Conclusion
It is clear that the array of competencies needed for success in a healthcare leadership role has grown exponentially more complex over the past decade. From social progress movements to extraordinarily sophisticated technological innovations in care, the world is rapidly transforming, and the healthcare sector is no exception.
The core competencies of workforce development and diversity, public health and preparedness skills, and regulatory and policy acumen are best developed with a combination of experiential and classroom-based knowledge. A mentor, too, can be an invaluable resource to support healthcare leaders as they navigate this turbulent, dynamic, and exciting sector.

